TABLE OF CONTENTS
2. Structure and Function of the Intestinal Barrier
- 3.1. The Chemical Barrier
- 3.2. The Physical Barrier
- 3.3. The Immune Barrier
4. Underlying Causes of a Leaky Gut
5. Potential Health Consequences Associated with a Leaky Gut
- 6.1. Urine
- Lactulose Mannitol
- 6.2. Serum
- Lipopolysaccharide
- Zonulin or Zonulin/Occludin
- Citrulline
- Intestinal Fatty Acid Binding Protein
- 6.3. Fecal
- Secretory IgA
7. Exploring Nutrients to Support Healthy Gut Function‡
- Glutamine
- Botanicals
- Probiotics & Prebiotics
- Zinc Carnosine
- Deglycyrrhizinated Licorice (DGL), Marshmallow Root & Slippery Elm
8. Pure Encapsulations® Nutrient Solutions
- Betaine HCl
- Digestive Enzymes Ultra
- MotilPro
- MicroDefense w/ Oregano
- Probiotic G.I.
- Poly-Prebiotic Powder
- Peptic-Care‡
- Epi-Integrity Powder
- L-Glutamine
- SunButyrateTM-TG liquid
- DGL Plus®
THE FIRST LINE OF DEFENSE
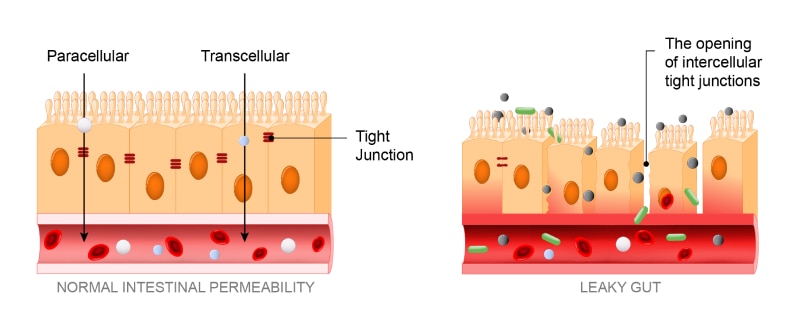
This small intestinal barrier is the first line of defense when it comes to living organisms. It is not only responsible for absorbing nutrients from the diet but also serves a pivotal role as the body’s first line of defense against ingested harmful substances. Only a single layer of cells protects the body from the external world, and it exists in this barrier. A healthy and properly functioning intestinal barrier protects from non-beneficial microorganisms, undigested food particles and toxins from entering the bloodstream. When the integrity of the intestinal barrier is disrupted, it can become hyperpermeable.
Intestinal hyperpermeability, also known as Leaky Gut, allows non-beneficial microorganisms, toxins and undigested food particles to “leak” through the barrier and into circulation, where they can impact other organs and systems.
STRUCTURE AND FUNCTION OF THE INTESTINAL BARRIER
Homeostasis of the intestinal barrier relies on three interdependent layers: a chemical barrier, a physical barrier and an immune barrier.
CHEMICAL BARRIER
The chemical barrier consists of the microbiota-rich mucus layer. In direct contact with the contents of the lumen, it’s the body’s first line of defense and provides a protective coating over epithelial cells. Surrounding cells secrete glycoproteins, mucin, and peptides to support the health of the mucus layer and prevent bacteria, toxins and antigens from penetrating the epithelial layer. Secretory IgA is also found in the mucus, as it helps prevent bacteria from adhering to the epithelial cells.
The mucus layer is also home to the microbiota of the gut. The microbiota participates in many important roles that regulate barrier function and overall health, including harvesting nutrients from the diet, synthesizing vitamins and metabolites like short-chain fatty acids, preventing the proliferation of non-beneficial bacteria and engaging in crosstalk with other organs and systems. Aberration of the gut microbiota and its metabolites can lead to downstream consequences and alterations of the intestinal barrier.1
PHYSICAL BARRIER
Beneath the mucosa exist multiple cell types, including enterocytes, goblet cells, enteroendocrine cells, Paneth cells and intestinal stem cells. These cells are responsible for assisting with the absorption of nutrients and interacting with immune cells, the mucus layer and the microbiota to support homeostasis. Collectively, these cells form the one-cell-thick, semipermeable physical barrier known as the epithelial intestinal barrier. The epithelial cells tightly regulate the space between cells (paracellular) and through cell (transcellular) permeability. The integrity of the epithelial barrier is maintained by tight junctions, which are key structures that seal and provide tight connections between the adjacent cells and regulate paracellular trafficking of macromolecules through the intestinal barrier. The overlapping of proteins like zonulin, occludin, clauden and cadherin provides stability of tight junctions. Changes to the structure or function of these proteins are implicated in leaky gut.2, 3, 4
IMMUNE BARRIER
Beneath the epithelial barrier is the lamina propria, comprised of innate and adaptive immune cells, making up the immune barrier. Also residing here are components of the mucosal- associated lymphoid tissue (MALT) and gut-associated lymphoid tissue (GALT) and include Peyer’s Patches, which support IgA’s production and transport between the interdependent layers. Macrophages, dendritic cells, T cells, B cells and mast cells also colonize the immune barrier.
WHAT CAN GO WRONG?
Interferences in the structure and functions of this cellular barrier, or its chemical and immune components, can lead to increased permeability. Intestinal hyperpermeability, also known as leaky gut, allows non-beneficial microorganisms, toxins and undigested food particles to “leak” through the barrier and into circulation, where they can impact other organs and systems.
UNDERLYING CAUSES OF A LEAKY GUT
Patients with gut barrier concerns and intestinal hyperpermeability may present uniquely different symptoms. This occurs because individuals may encounter a variety of factors throughout their lifetime that can lead to leaky gut, including:
- Food sensitivities3
- Stress5
- Mast cell activation6, 7
- Poor diet or alcohol intake8, 9
- Inadequate zinc or Vitamin D10, 11
- Certain medications12, 13
- Non-beneficial microorganisms,14
- Environmental contaminants
- Altered microbiome2
- Low digestive enzymes or HCl
POTENTIAL HEALTH CONSEQUENCES ASSOCIATED WITH A LEAKY GUT
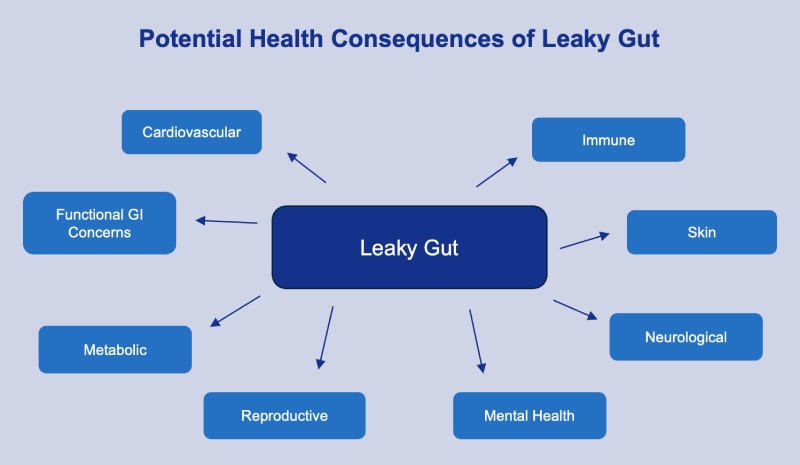
Optimizing the function and integrity of the intestinal barrier can be one of the most important things a practitioner can do for their patient. The consequences of a leaky gut can extend far beyond the gut and impact many areas of health, including cardiovascular,15 metabolic,16, 17 mental,18, 19 neurological,20 skin,21 immune22 and reproductive health.
ASSESSMENTS FOR LEAKY GUT
URINE
Lactulose Mannitol: One of the initial non-invasive laboratory tests, the lactulose mannitol test uses sugar molecules to assess intestinal permeability. The patient is given an oral dose of both lactulose and mannitol. the smaller monosaccharide, freely passes through the epithelial barrier and into the bloodstream. Lactulose, a larger disaccharide, is typically prevented from paracellular travel through the tight junctions. The presence of these two sugar molecules in the urine is expressed as a ratio of the percentage of the ingested doses, known as the LMR or lactulose mannitol ratio. This ratio can reflect increased intestinal permeability.24
SERUM
Lipopolysaccharide: Lipopolysaccharide, or LPS, is an endotoxin found in the cell wall of Gram-negative organisms that is naturally present in the gastrointestinal, respiratory and genitourinal tracts. When the organism’s outer membrane is shed or ruptured, LPS is expressed. The detection of LPS and LPS IgA, IgG and IgM antibodies in the serum can indicate intestinal permeability.23 Because other factors can cause LPS to be present in the serum, LPS testing is often used alongside other biomarkers for leaky gut.
Zonulin or Zonulin/Occludin: These proteins contribute to the stability of tight junctions and epithelial cells and their presence in the serum can be clinically relevant when assessing intestinal permeability.24
Citrulline: Citrulline is an amino acid synthesized by enterocytes from glutamine or arginine. Traditionally used as a marker for decreased enterocyte mass with immune-related conditions of the GI tract, low plasma citrulline can also be a significant biomarker of intestinal barrier permeability.
Intestinal Fatty Acid Binding Protein (I-FABP): Plasma I-FABP is another useful biomarker for assessing intestinal permeability. Expressed by the enterocytes, I-FABP belongs to a family of fatty acid-binding proteins responsible for binding to and transporting fatty acids.24 Like other markers for leaky gut, I-FABP is detected in the serum when it has breached the intestinal barrier due to hyperpermeability.24 In a case-control study by Linsalata et al., higher serum levels of I-FABP were detected in patients with Functional GI Concerns with occasional diarrhea, concurrent with altered lactulose-mannitol ratio and increased intestinal permeability.25
FECAL
Secretory IgA: Found throughout the mucosa of the intestinal barrier, sIgA supports the mucosa’s
health by preventing bacteria adhesion to the epithelial cells and coordinating immune responses.24 Secretory IgA found in the stool can suggest hyperpermeability. Also detected in saliva and serum, sIgA
testing is often interpreted alongside other biomarkers for leaky gut.
According to a survey conducted in
2022 by the American Gastroenterological Association, 1 in 4 people in the US experience occasional
uncomfortable gut symptoms over the last year.26 As the list of health conditions associated with
leaky gut continues to grow, optimizing a patient’s gut function to maintain their overall health should take
center stage. Just as leaky gut has no single cause, there is no single cookie-cutter approach. Many
practitioners find that their patients with leaky gut benefit from a customized plan, using the 5R Program as a
guide.
EXPLORING NUTRIENTS TO SUPPORT HEALTHY GUT FUNCTION‡
Along with dietary and lifestyle changes, nutrients that support GI motility, gut barrier integrity and microbial balance can help support patient outcomes.
Glutamine: The most abundant amino acid in the body is a primary energy source for intestinal epithelial cells and is utilized by the body for tissue repair and gastrointestinal support.27, 28, 29 Glutamine plays a large role in maintaining healthy intestinal integrity by enhancing the intestine’s protective mucosal lining.‡
Botanicals: Some patients may benefit from artemisia, olive leaf extract, oregano, clove or berberine sulfate, which can help promote healthy microbial balance.30, 31, 32, 33, 34‡
Probiotics & Prebiotics: Probiotics have been shown to be efficacious in all subtypes of
Functional GI Concerns, although specific strains should be considered for each subtype and symptoms presented.
Overall, meta-analyses have shown that probiotics may significantly improve stool consistency, regulate stool
frequency and gut transit time.35, 36, 37‡
Prebiotic fibers, like Arabinogalactan, are
nondigestible food components that modulate and support the gut microbiota. They perform beneficial metabolic,
trophic and protective functions within the gut, leading to overall cellular, immune and metabolic
support.38 Arabinogalactan may increase the concentration of beneficial bacteria, such as
Bacteroidetes and Faecalibacterium prausnitzii.39‡
Zinc carnosine: Zinc and carnosine provide synergistic antioxidant protection, support the stomach’s mucosal defenses, buffer gastric acid and maintain healthy cytokine release.40 Studies suggest that this combination is more effective in maintaining the integrity of the gastric lining than either ingredient alone.41‡
Deglycyrrhizinated licorice (DGL), Marshmallow Root & Slippery Elm: Deglycyrrhizinated licorice (DGL), marshmallow root and slippery elm bark are demulcent herbs that are traditionally recognized for their value in soothing the gastrointestinal tract and maintaining the integrity of the mucosal lining.42, 43, 44‡
PURE ENCAPSULATIONS® NUTRIENT SOLUTIONS
Pure Encapsulations® provides products designed to complement your care plans for patients needing digestive and GI support. You’ll find Pure Encapsulations offers nutrients individually and in combination to meet all your patient’s unique needs. Pure Encapsulations® products are also highly suitable for use with the 5R Program, a functional medicine model.
DIGESTIVE ENZYMES
- Betaine HCl contains betaine HCl and pepsin to support healthy gastric function and promote absorption of protein, vitamin B12, and calcium.‡ Suggested use: 1 capsule, 3 times daily, with each meal.
- Digestive Enzymes Ultra contains an extensive profile of vegetarian digestive enzymes to support protein, carbohydrate, fat, fiber, and dairy digestion and promote enhanced nutrient bioavailability and absorption.‡ Suggested use: 2 capsules with each meal.
MOTILITY
- MotilPro contains ginger extract, 5 hydroxytryptophan, pyridoxal-5 phosphate, and acetyl-l-carnitine that provides support for gastrointestinal motility, GI comfort and stimulation of gut-signaling neurons.‡ Suggested use: 2 capsules, 1-2 times daily between meals.
MICROBIAL BALANCE
- MicroDefense w/ Oregano is comprised of a combination of olive leaf, artemisia and clove extracts to promotes healthy gastrointestinal tract function and microbial balance‡ and supports immune function and respiratory tract balance.‡ Suggested use: 1 capsule, 1-3 times daily, just before a meal, with 6-8 oz water for 2-3 months.
PROBIOTICS & PREBIOTICS
- Probiotic G.I. provides 10 billion CFU per capsule of the beneficial bacteria Lactobacillus acidophilus, Lactobacillus salivarius, Lactobacillus casei, Bifidobacterium bifidum, Bifidobacterium lactis and Streptococcus thermophilus to promote healthy immune balance within the G.I. tract and help maintain the integrity of the intestinal mucosa.‡ Suggested use: 1 capsule, 1-2 times daily, with or between meals.
- Poly-Prebiotic Powder is a unique powdered blend of researched prebiotic fibers and polyphenols to support gastrointestinal, cellular and immune function by boosting Bifidobacteria and microbiome diversity.‡ Suggested use: 1 scoop, 1-2 times daily, mixed with a beverage or into food.
GUT BARRIER INTEGRITY
Peptic-Care‡ contains a patented 1:1 chelate of zinc and l-carnosine, providing synergistic GI mucosal protection and supports the stomach’s mucosal defenses, buffers gastric acid, maintains healthy cytokine release and provides antioxidant support for the GI tract.‡ Suggested use: Take 1 capsule, 1-2 times daily with meals.
Epi-Integrity Powder promotes healthy modulation of mucosal immune responses to support GI integrity.‡ Suggested use: 1 scoop, 1-2 times daily. Add 1 serving to 8 oz of water or juice and shake or stir until dissolved.
L-Glutamine delivers 850 mg of L-glutamine to support the mucosal lining and healthy functioning of the gastrointestinal tract; it may help to maintain lean muscle mass.‡ Suggested use: 1 capsule, 1-3 times daily, between meals. Also available in powder.
SunButyrateTM – TG liquid provides 875 mg of short-chain fatty-acid butyric acid in one teaspoon to promote gut-barrier integrity, cytokine balance in the GI tract, abdominal comfort and bowel motility.‡ Suggested use: 1 teaspoon, 1-3 times daily, with meals.
DGL Plus® contains a synergistic combination of deglycyrrhizinated licorice extract, aloe vera extract, slippery elm and marshmallow root extract to help stimulate the quality and production of stomach mucus, provide nutritional support to the gastrointestinal tract and support the body’s natural defense mechanisms.‡ Suggested use: Take 1 capsule daily before a meal.
CONCLUSION
With the gut being the chief portal for entry of nutrients, antigens and non-beneficial microorganisms into the body, a healthy intestinal barrier is key to maintaining a healthy gut and overall health. A patient-centered approach with nutrient and lifestyle solutions tailored to an individual’s unique clinical presentation and nutrient needs can have a profound effect not just in the gut but at a systemic level.
With Pure Encapsulations, you have the promise of premium sourced ingredients backed by verifiable science, so you can be confident you are recommending products with quality, purity and potency.
RESOURCES
A Comprehensive Approach to Maintaining Normal Gut Health: Offers guidance and product suggestions for the 5R Program to address Leaky Gut Factors and other GI conditions, developed by the Institute for Functional Medicine.
Drug-Nutrient Interactions Checker | DNI Calculator: Offers scientifically supported, clinically relevant information that’s easy to understand with product suggestions based on verifiable science.
You can also explore Pure Encapsulations® to find On-Demand Learning, Clinical Protocols and other resources developed with our medical and scientific advisors.
REFERENCES
- Su Q, Tun HM, Liu Q, et al. Gut Microbes. 2023;15(1):2157697. doi:10.1080/19490976.2022.2157697
- Vita AA, Zwickey H, Bradley R. Front Nutr. 2022;9:962093. Published 2022 Sep 6. doi:10.3389/fnut.2022.962093
- Awad K, Barmeyer C, Bojarski C, et al. Cells. 2023;12(2):236. Published 2023 Jan 5. doi:10.3390/cells12020236
- Zhou Q, Zhang B, Verne GN. Pain. 2009;146(1-2):41-46. doi:10.1016/j.pain.2009.06.017
- Vanuytsel T et al. Gut. 2014;63(8):1293-1299. doi:10.1136/gutjnl-2013-305690
- Bashashati M et al. Neurogastroenterol Motil. 2018;30(1):10.1111/nmo.13192. doi:10.1111/nmo.13192
- Lee H et al. J Neurogastroenterol Motil. 2013;19(2):244-250. doi:10.5056/jnm.2013.19.2.244
- Saffouri GB et al. Nat Commun. 2019;10(1):2012. Published 2019 May 1. doi:10.1038/s41467-019-09964-7
- Bhonchal S et al. J Gastroenterol Hepatol. 2008;23(7 Pt 2):e43-e48. doi:10.1111/j.1440-1746.2007.05080.x
- Wessells KR et al. J Pediatr Gastroenterol Nutr. 2013;57(3):348-355. doi:10.1097/MPG.0b013e31829b4e9e
- Linsalata M et al. Nutrients. 2021;13(3):1011. Published 2021 Mar 21. doi:10.3390/nu13031011
- Duan H et al. Crit Rev Food Sci Nutr. 2022;62(6):1427-1452. doi:10.1080/10408398.2020.1843396
- Matsui H. et al. J Clin Biochem Nutr. 2011;48(2):107-111. doi:10.3164/jcbn.10-79
- Fukuda, Y et al. Digestion, 63(1), 93–96. doi:10.1159/000051918
- Kavanagh K, Hsu FC, Davis AT, Kritchevsky SB, Rejeski WJ, Kim S. Geroscience. 2019;41(6):923-933. doi:10.1007/s11357-019-00112-z
- De Munck TJI, Xu P, Verwijs HJA, et al. Liver Int. 2020;40(12):2906-2916. doi:10.1111/liv..14696
- Damms-Machado A, Louis S, Schnitzer A, et al. Am J Clin Nutr. 2017;105(1):127-135. doi:10.3945/ajcn.116.131110
- Asbjornsdottir B, Snorradottir H, Andresdottir E, et al. Nutrients. 2020;12(7):1982. Published 2020 Jul 3. doi:10.3390/nu12071982
- Maes M, Kubera M, Leunis JC. Neuro Endocrinol Lett. 2008;29(1):117-124.
- Clairembault T, Leclair-Visonneau L, Coron E, et al. Acta Neuropathol Commun. 2015;3:12. Published 2015 Mar 10. doi:10.1186/s40478-015-0196-0
- Nam B, Kim SA, Park SD, et al. PLoS One. 2020;15(4):e0231268. Published 2020 Apr 10. doi:10.1371/journal.pone.0231268
- Zheng Y, Zhang Z, Tang P, et al. Front Immunol. 2023;14:1143548. Published 2023 Apr 24. doi:10.3389/fimmu.2023.1143548
- Nendl A, Raju SC, Broch K, et al. Front Cardiovasc Med. 2023;10:1160030. Published 2023 Jun 2. doi:10.3389/fcvm.2023.1160030
- Linsalata M, Riezzo G, D’Attoma B, Clemente C, Orlando A, Russo F. BMC Gastroenterol. 2018;18(1):167. Published 2018 Nov 6. doi:10.1186/s12876-018-0888-6
- American Gastroenterological Association. Accessed January 22, 2024.
- Rastgoo S, Ebrahimi-Daryani N, Agah S, et al. Front Nutr. 2021;8:746703. Published 2021 Dec 16. doi:10.3389/fnut.2021.746703
- Sasaki E, et al. Luminescence. 2013 Jul- Aug;28(4):442- 9.
- Song QH, et al. Int J Clin Pharmacol Ther. 2015 May;53(5):372-6
- Oguche S, et. al. Am J Trop Med Hyg. 2014 Nov;91(5):925-35
- Takeda R, et. al. Phytomedicine. 2013 Jul 15;20(10):861-4.
- Force M, et al. Phytother. Res. 2000: 14, 213–214.
- Bansal V, et. al. Niger Med J. Nov-Dec 2019;60(6):285- 289.
- Khin-Maung-U, et. al. Br Med J (Clin Res Ed). 1985 Dec 7;291(6509):1601-5.
- Yong Wen, Jun Li, Qing Long, Chao-chi Yue, Bing He, Xue-gui Tang,
- International Journal of Surgery, 2020. Volume 79. pp 111-19.
- Sun JR, Kong CF, Qu XK, Deng C, Lou YN, Jia LQ Saudi J Gastroenterol. 2020;26(2):66-77. doi:10.4103/sjg.SJG_384_19
- Shang X, E FF, Guo KL, et al. Nutrients. 2022;14(12):2482. Published 2022 Jun 15. doi:10.3390/nu14122482
- Natalia S, et al. Nutrients. 2018 May; 10(5): 576.
- Riede L, et. al. Curr Med Res Opin. 2013 Mar;29(3):251-8.
- Shimada T, et al. J Pharmacol Exp Ther. 1999 Oct;291(1):345-52.
- Sakae K, et al. Nutr Clin Pract. 2013 Oct;28(5):609-16.
- Das SK, et al. J Assoc Physicians India. 1989 Oct;37(10):647.
- Deters A, et al. J Ethnopharmacol. 2010 Jan 8;127(1):62-9.
- Marakis G, et al. Phytomedicine. 2002 Dec;9(8):694-9.







