TABLE OF CONTENTS
1. Thyroid Health: Functions and Common Symptoms
2. Thyroid Hormone Metabolism: Looking at the Whole Pathway
3. Inhibitors of T4 to T3 Conversion
- 3.1. Free T3 and Free T4
- 3.2. Reverse T3
- 3.3. Thyroid Antibodies
- 3.4. Adrenal Panel
5. Nutrients to Support Thyroid Function‡
6. Pure Encapsulations® Nutrient Solutions
Standard assessments may overlook factors that underlie a patient’s thyroid concerns. Learn more about looking beyond TSH and T4 to support your patient’s thyroid hormone metabolism and overall health.
THYROID HEALTH: FUNCTIONS AND COMMON SYMPTOMS
An optimally functioning thyroid is essential for maintaining body homeostasis. Thyroid hormones influence nearly every organ system in the body, encompassing the heart, central nervous system, autonomic nervous system, skeletal structure, gastrointestinal tract, and metabolism.
The rate of thyroid concerns has more than doubled in the past twenty years, with women affected at a prevalence five to eight times that of men.1, 2 More than half of individuals with symptoms are unaware they are related to their thyroid.1 Thyroid symptoms can vary between individuals and can include:
- Fatigue
- Occasional constipation
- Weight gain, difficulty losing weight
- Intolerance to cold, cold hands and feet
- Dry skin
- Dry, thinning hair or hair loss
- Mood concerns
- Joint and muscle discomfort
- Heavy or irregular menstrual cycles, fertility concerns
- Slowed heart rate
- Low libido
THYROID HORMONE METABOLISM: LOOKING AT THE WHOLE PATHWAY
Four hormones have been identified to be secreted by the thyroid, T1, T2, T3, and T4. The two primary hormones are thyroxine (T4), a prohormone, and triiodothyronine (T3), which is 300 times more biologically active than T4.3
Once T4 is secreted, it is bound to transport proteins and carried to the cells and tissues where it passes through a series of metabolic transformations and is either converted to T3 or inactivated into reverse T3 (rT3). T3 is utilized by mitochondria and contributes to metabolism of glucose and lipids, regulates metabolic responses according to energy intake, controls thermogenesis and basal and oxidative metabolism—essentially affecting all tissues in the body.4
Successful conversion of T4 to T3 relies heavily on transport proteins, along with nuclear receptors and selenium-dependent enzymes known as deiodinases. These three players are crucial to homeostasis at the cellular level as they coordinate the uptake, activation and deactivation of thyroid hormone within the cell.5 Conversion of T4 to T3 occurs primarily in the liver and kidneys, but also within the gut, bones, muscles, adipose tissue, heart and CNS.6, 7, 8
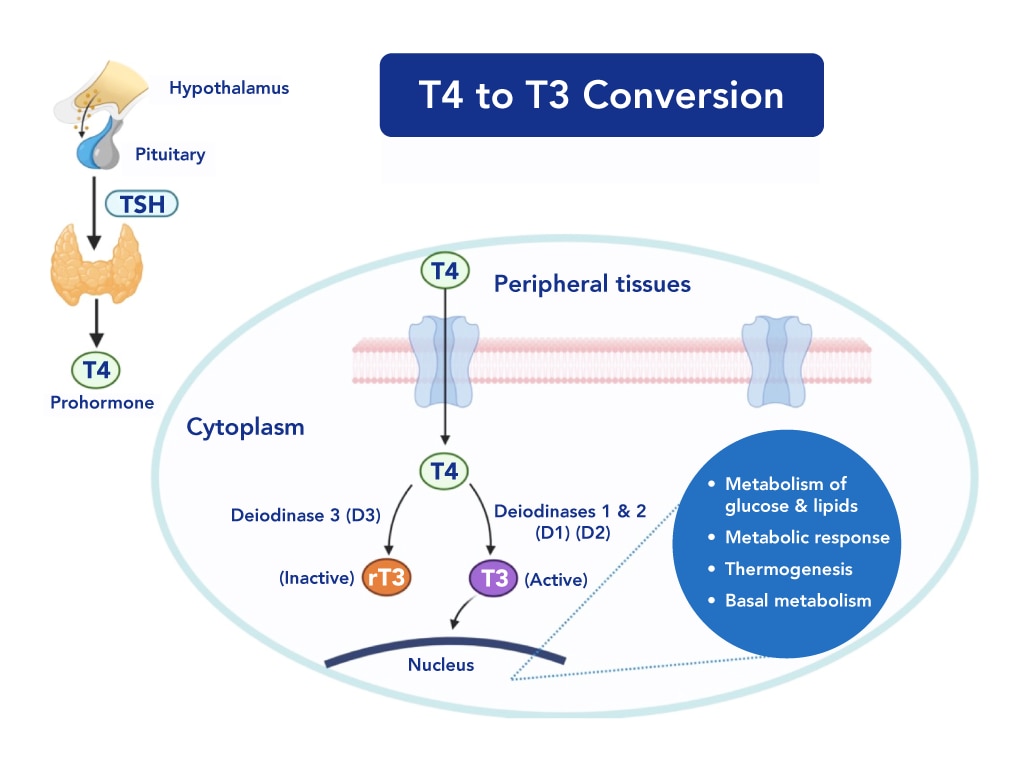
Created with BioRender.com
INHIBITORS OF T4 TO T3 CONVERSION
Eighty percent of the T3 found in circulation is produced by peripheral conversion from T4.4 A number of lifestyle, environmental, and dietary factors can inhibit this conversion and lead to symptoms.4, 9, 10, 11, 12
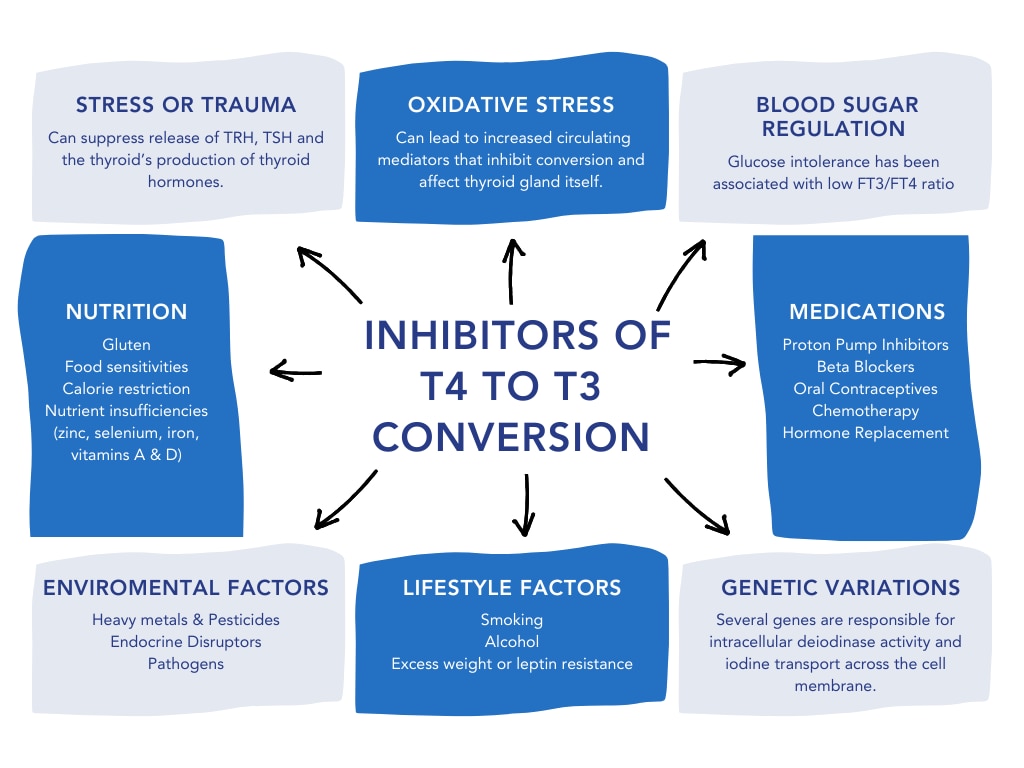
T4 to T3 conversion influences all tissues within the body, as they are dependent on T3 for normal cell function.4
LOOKING BEYOND TSH AND T4
In line with standard practices, practitioners commonly rely on TSH and T4 levels to screen for thyroid concerns. While these markers play important roles, they don’t tell the whole story. Getting to the root of an individual’s symptoms requires investigating what is occurring further down the thyroid hormone pathway at the cellular level, and why. This begins with understanding that although TSH and T4 levels can provide insight into thyroid gland function, they don’t reflect:
- Alterations in cellular sensitivity to thyroid hormones
- Inadequate peripheral conversion of inactive T4 to metabolically active T3
- Poor uptake of thyroid hormones into the mitochondria
- Activity of rT3, anti-thyroid antibodies or environmental factors which can displace thyroid hormones and prevent their binding to cellular receptors.
Any one of these factors along with impaired T4 to T3 conversion, or fluctuation in T3 and rT3 levels can trigger changes in an individual long before TSH or T4 are outside their respective reference ranges.
Expanding the assessment of thyroid function beyond TSH and T4 can provide insight into what is happening peripherally to T4.
The following markers can provide evidence of suboptimal thyroid function:
FREE T3 AND FREE T4
Measuring total thyroid hormones provides the sum of both the free thyroid hormone and thyroid hormone bound to a protein; however, it does not differentiate how much of that hormone is available for uptake by the cells. A hormone bound to a protein is inactive. Only the free T4 and free T3 tests measure the levels of thyroid hormones in circulation that are available to cells.
REVERSE T3
rT3 can be produced in response to physical or emotional stress. Free T3 and rT3 can both bind to thyroid receptors on the cell. When rT3 binds to thyroid receptors, it inactivates them and prevents the metabolically active hormone T3 from binding to receptors.
THYROID ANTIBODIES
Thyroid peroxidase antibodies (TPO antibodies) and thyroglobulin antibodies (TG antibodies) can be produced when the body begins to lose “self-tolerance”. Thyroid antibodies can be present long before aberrations are seen in TSH and T4.
ADRENAL PANEL
Elevated urinary cortisol metabolites have been associated with diminished peripheral thyroid hormone metabolism.14 Examining the role stress plays in thyroid function in each patient is foundational for any thyroid care plan.
NUTRIENTS TO SUPPORT THYROID FUNCTION
Various nutrients participate in the synthesis, metabolism, and mechanisms of action of thyroid hormones.
Curcumin helps to neutralize free radicals that may affect iodothyronine 5’-monodeiodinase enzyme activity, the limiting factor in the conversion of T4 to the more active T3 hormone.14‡
Vitamins A and D help to maintain healthy thyroid cell metabolism and support triiodothyronine (T3) and thyroxine (T4) hormone function.15, 16
Ashwagandha helps maintain healthy thyroid function and relaxation as suggested in preliminary research.17‡
Forskolin in coleus extract has been shown to support thyroid hormone metabolism in preclinical models, potentially by promoting adenylate cyclase activity.18‡
Zinc and Selenium help to maintain healthy thyroid cell metabolism and support triiodothyronine (T3) and thyroxine (T4) hormone function.19, 20 Selenium has also been shown to help to neutralize free radicals that may affect iodothyronine 5’-monodeiodinase enzyme activity, the limiting factor in the conversion of T4 to the more active T3 hormone.13‡
Probiotics support healthy intestinal microflora to promote digestive and immune health.‡
PURE ENCAPSULATIONS® NUTRIENT SOLUTIONS
Pure Encapsulations® offers high-quality supplements that are FREE FROM unnecessary additives and many common allergens for patients who may need thyroid and overall health support. You’ll find Pure Encapsulations® offers nutrients individually and in combination to meet all your patients’ unique needs.
COMPREHENSIVE SUPPORT
- Thyroid Support Complex‡ is a comprehensive thyroid support formula that contains vitamins, minerals, and herbal extracts to nourish and support thyroid gland function.‡ Suggested use: Take 2 capsules daily, with a meal.
IMMUNE SUPPORT
- Zinc 30 provides broad physiological support including immune function and emotional wellness.‡ Suggested use: Take 1 capsule, 1-2 times daily, with meals.
- Selenium (citrate) supports antioxidant defenses and cellular health and provides immune system support.‡ Suggested use: Take 1 capsule daily, with a meal, or as directed by a health professional.
- Vitamin D3 125 mcg (5,000 IU) supports musculoskeletal, cardiovascular, neurocognitive, cellular, and immune health.‡ Suggested use: Take 1-5 capsules daily, or as directed by a health professional. Consume with food.
DETOXIFICATION SUPPORT
- Curcumin 500 with Bioperine® supports the body’s natural detoxification system and helps maintain healthy hepatic function. Helps maintain healthy cell cycle function and supports antioxidant defenses.‡ Suggested use: Take 1 capsule, 1-3 times daily, between meals.
MICROBIAL BALANCE
- Probiotic 50B offers seven researched probiotic strains that promote healthy intestinal ecology to support gastrointestinal and immune health.‡ Suggested use: Take 1 capsule daily, with or between meals.
SUMMARY
Environmental, genetic, lifestyle, and nutritional factors can affect the thyroid hormone pathway in different ways for different individuals. While laboratory tests can be critical tools, the absence of markers mentioned in thyroid testing does not equate to optimal function.
Personalized medicine addresses the whole person, which requires exploration of the unique mediators, triggers, and antecedents that may be impacting each patient’s thyroid hormone function and presenting symptoms.
RESOURCES
Thyroid Support Protocol: Developed in collaboration with our scientific and medical advisors to support thyroid health.‡
Drug-Nutrient Interactions Checker: Offers scientifically supported, clinically relevant information along with relevant product suggestions.
You can also explore Pure Encapsulations® to find On-Demand Learning, Clinical Protocols, and other resources developed with our medical and scientific advisors.
REFERENCES
- American Thyroid Association. Accessed on March 18, 2024.
- Wyne KL, Nair L, Schneiderman CP, et al. J Endocr Soc. 2022 Nov 10;7(1):bvac172. doi: 10.1210/jendso/bvac172.
- Abdalla SM, Bianco AC. Defending plasma T3 is a biological priority. Clin Endocrinol (Oxf). 2014;81(5):633-641. doi:10.1111/cen.12538
- Severo JS, Morais JBS, de Freitas TEC, et al. The Role of Zinc in Thyroid Hormones Metabolism. Int J Vitam Nutr Res. 2019;89(1-2):80-88. doi:10.1024/0300-9831/a000262.
- Sabatino L, Lapi D, Del Seppia C. Factors and Mechanisms of Thyroid Hormone Activity in the Brain: Possible Role in Recovery and Protection. Biomolecules. 2024;14(2):198. Published 2024 Feb 7. doi:10.3390/biom14020198
- Sabatino L, Vassalle C, Del Seppia C, Iervasi G. Deiodinases and the Three Types of Thyroid Hormone Deiodination Reactions. Endocrinol Metab (Seoul). 2021;36(5):952-964. doi:10.3803/EnM.2021.1198
- Fröhlich E and Wahl R. Trends Endocrinol Metab. 2019 Aug;30(8):479-490. doi: 10.1016/j.tem.2019.05.008. Epub 2019 Jun 27. PMID: 31257166.
- Samuels, MH. J Clin Endocrinol Metab. 2008. 85(4):1388-93.
- Mancini A, Di Segni C, Raimondo S, et al. Mediators Inflamm. 2016;2016:6757154. doi:10.1155/2016/6757154
- Roti E et al. Int J Obes Relat Metab Disord. 2000;24 Suppl 2:S113-S115. doi:10.1038/sj.ijo.0801293
- Farasat T et al. Journal of Diabetes and its Complications. 2012. 26(6):522-25. doi:10.1016/J.JDIACOMP.2012.05.017
- Gillam MP et al. Curr Opin Pediatr. Aug 2001.13(4):364-72. doi: 10.1097/00008480 200108000 00014. PMID: 11717564.
- Vantyghem MC et al. J Endocrinol Invest. 1998.21(4): 219-25.
- Mahmoodianfard S et al. J Am Coll Nutr. 2015;34(5):391-9.
- Farhangi MA et al. J Am Coll Nutr. 2012. Aug;31(4):268-74.
- Mazokopakis EE et al. Hell J Nucl Med. 2015.18(3):222-27.
- Chandrasekhar K et al. Indian J Psychol Med. 2012. Jul-Sep; 34(3): 255–262.
- Godard MP et al. Obes Res. 2005 Aug;13(8):1335-43.
- Kilic M. Neuro Endocrinol Lett. 2007 Oct;28(5):681-5.
- Combs GF Jr et al. Am J Clin Nutr. 2009 Jun;89(6):1808-14.







